Australia needs tougher laws to protect consumers from unexpected bills in the private health system, where 60 percent of all elective surgical procedures occur, the peak body for private health funds say.
Private Healthcare Australia (PHA) is calling on the Albanese Government to ensure consumers are not held liable for any costs that are not disclosed up-front before their medical treatment, with civil and criminal penalties for breaches.
The call comes as new data shows the median out-of-pocket cost for Australians having common procedures funded by their health insurance have increased up to 300 percent over the past five years. The biggest increases have occurred in hospital fees for heart angiogram procedures and gastroscopies (investigations of the upper digestive tract) where the median out-of-pocket fee has surged from $50 in 2017-18 to $200 in 2022-23.
In a concerning emerging trend, some procedures that previously attracted no out-of-pocket charges have started attracting these costs in recent years. For example, in 2017-18 most procedures had no out-of-pocket fee for cataract surgery or a cystoscopy (an investigation of the bladder). They now attract a $100 and $200 median out-of-pocket fee respectively.
PHA CEO Dr Rachel David said there is currently no way of knowing if these out-of-pocket costs were fully disclosed to consumers before they had their procedures, however anecdotal reports suggest some people are still getting shocked by bills worth hundreds of dollars after their treatment. These bills can come from the hospital, medical specialists, or pathology and diagnostic services they encountered.
“Australia needs to follow international best practice and introduce tough laws to protect consumers from surprise billing for healthcare services. For example, there was bipartisan political support for the ‘No Surprises Act’ in the US, where consumers can confidently proceed with healthcare knowing they won’t get a financial shock at the end,” she said.
“Fifty-five percent of Australians are paying for private health insurance. These people are contributing to their own healthcare and taking pressure off our stressed public hospital system. They should be guaranteed protection from unanticipated costs.”
“Inevitably, some procedures may result in unexpected complications, but a proper informed financial consent process ensures patients are made aware of this possibility prior to surgery.”
“Ideally an up-front quote should be provided which includes all likely out-of-pocket costs from the providers involved in the patient’s care. If we can do it for car and home repairs, there is simply no valid reason why this can’t happen for medical treatment.”
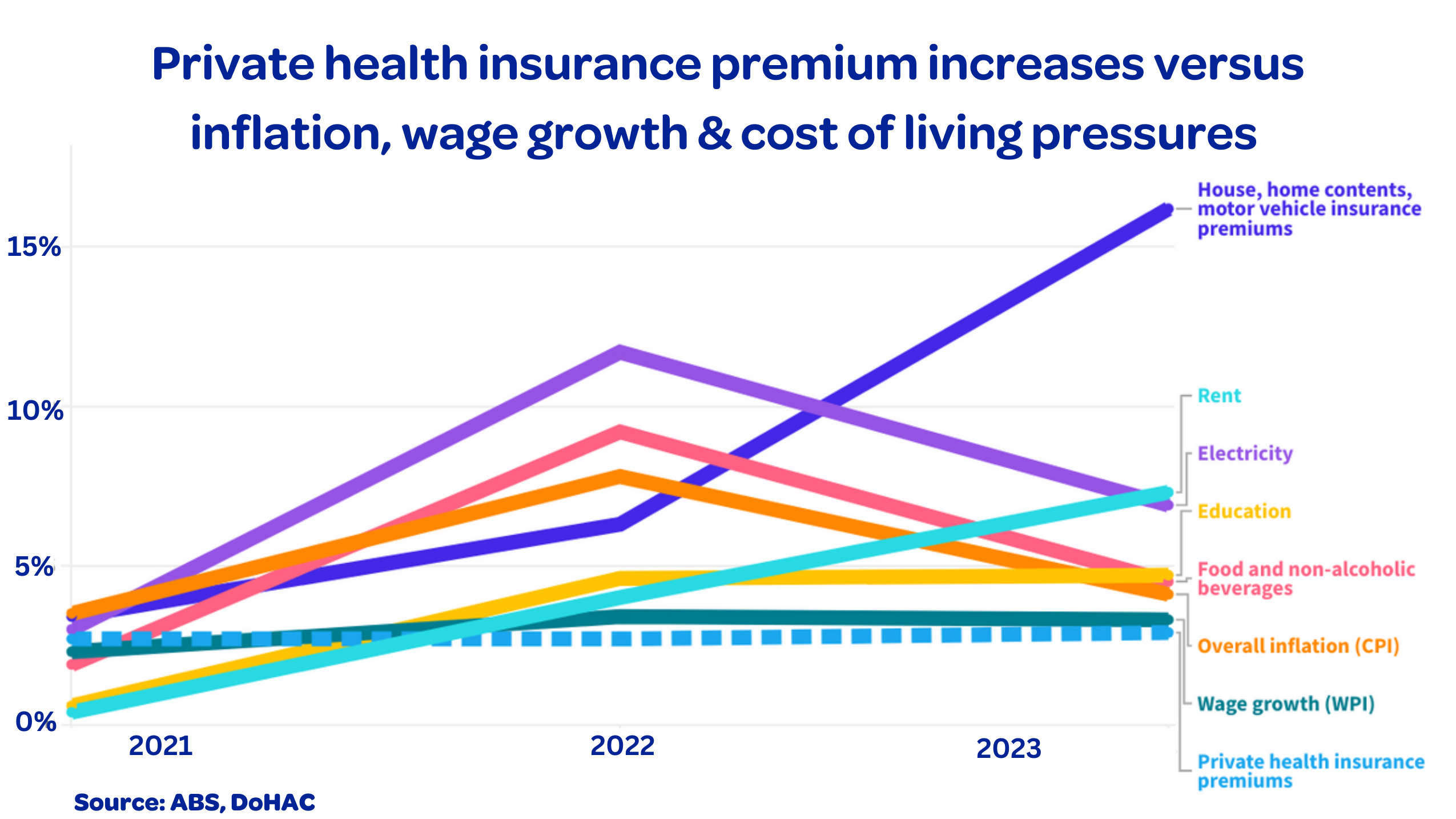
“In the current cost-of-living crisis, we must do everything we can to reduce the cost of medical treatment for Australians who are increasingly relying on private health insurance to get fast access to private healthcare and avoid public hospital waiting lists.”
Most hospitals have entered agreements with health funds to reduce out-of-pocket costs for their customers. Recently, there has been a decline in patients with private health insurance treated in hospitals without an agreement. However, day hospitals are not on average moving with this trend. Day hospitals charge patients significantly higher out-of-pocket hospital fees than other private hospitals.
There are four major types of surprise billing:
- High out-of-pocket charges not disclosed beforehand.
- Split billing where the full cost of the service is not disclosed to various payers including the consumer, their health fund and Medicare.
- Charges that are related to the service but are not described as part of the service. For example, a doctor or hospital seeks to increase their income by charging a “booking” or an “administration” fee.
- Change of scope during service. For example, where a complication in surgery required an unexpected intervention. Appendix provides recent examples.
Private health insurance data on median out-of-pocket fees charged for the most common medical procedures funded by health insurance in private hospitals.
| Procedure |
Out-of-pocket cost 2017-18 |
Out-of-pocket cost 2022-23 |
Change (%) |
| Cataract surgery |
$0 |
$100 |
100-fold |
| Cystoscopy (bladder investigation) |
$0 |
$200 |
200-fold |
| Colonoscopy (bowel investigation) |
$200 |
$250 |
25 |
| Knee replacement surgery |
$600 |
$813 |
35 |
| Hip replacement surgery |
$669 |
$905 |
35 |
| Heart angiogram (heart investigation) |
$50 |
$200 |
300 |
| Transperineal prostate biopsy |
$395 |
$672 |
70 |
| Hysteroscopy (uterus investigation) |
$400 |
$750 |
87 |
| Gastroscopy (upper digestive tract investigation) |
$50 |
$200 |
300 |
Appendix: Billing behaviour examples
Example one
A surgeon charges a patient $500 out-of-pocket cost for a surgery, payable before the date of surgery. The surgeon then bills $600 for the surgery under a “no gap” agreement with the health fund, where Medicare pays $300 and the health fund pays $300. The patient does not receive another bill as it is handled by the health fund and the hospital.
Both Medicare and the health fund believe the patient has not paid a gap, and Medicare statistics record zero out-of-pocket costs. While government figures the costs of the surgery to be $600, the actual cost is $1100 with a large out-of-pocket payment. Under the proposed changes, this would not be legal and all amounts charged need to be disclosed to each payor.
Example two
A doctor tells the patient they are not charging a gap fee for a procedure and receives a larger rebate from the patient’s health fund. However, the surgical assistant charges a large out-of-pocket cost and splits the extra payment with the primary surgeon. Under the proposed changes, this would not be legal and all amounts received need to be disclosed to each payor.
Example three
A patient receives a bill from a surgical assistant but was not informed that there would be a surgical assistant for the procedure. Under the proposed changes, the patient would not be liable for any out-of-pocket costs for services where the service was predicted.
Example four
During surgery, the doctor discovers another problem which means the operation is much more complex than anticipated. In this instance, the patient is liable for additional costs.
Read PHA’s policy paper Combatting Surprise Billing in Australia here.
– ENDS –
Media contact: Jen Eddy, 0439 240 755
Back to topThe post Health funds call for ‘surprise billing law’ as new data reveals soaring out-of-pocket costs for medical procedures. first appeared on Private Healthcare Australia (PHA).